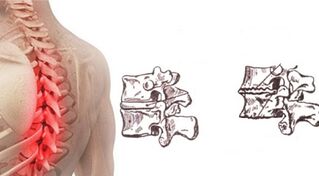
Thoracic osteochondrosis is rare in clinical practice. Previously, it was mainly diagnosed in the elderly, but is now often detected in patients under 35 years of age. More often, the pathology develops in women than in men. This degenerative-dystrophic disease is difficult to diagnose, as severe symptoms appear only in the later stages.
In addition, the symptoms of this disorder can easily be mistaken for signs of impaired lung and heart function. This disease cannot be left untreated as it can lead to curvature of the spine, the development of a persistent pain syndrome, and other complications that can negatively affect human quality of life.
What is thoracic osteochondrosis?

In the international classification of diseases, this pathological condition has an ICD-10 code - M42. Thoracic osteochondrosis is much less common than cervical or sacral. It's not by chance. Due to the presence of a rigid rib cage in this part of the body, this part of the spine is physiologically less mobile.
The thoracic region contains more vertebrae than the cervical and lumbar vertebrae, but in this part of the spine, the discs are thinner. These anatomical characteristics contribute to reducing the mobility of this part of the spine, making it less subject to injury.
However, when exposed to a number of adverse factors, osteochondrosis can develop. At first, there are signs of damage to a disc, but in the future, other elements may be involved in the pathological process. As the disease progresses, bone elements are damaged, as well as the ligaments and muscles that support the spine.
Degenerative-dystrophic processes in the thoracic region grow more slowly. It is not uncommon for years to pass before the fibrous rings of damaged discs are destroyed so much that bulges and hernias appear.
Serious clinical manifestations occur after a critical decrease in disc height and root entrapment. This can lead not only to dorsago, that is, short-term pain attacks in the thoracic region, but also to a violation of the innervation of internal organs. Pinched nerve roots that extend into this area are much more difficult to treat.
Development reasons
In most cases, column problems do not appear suddenly. A disease such as osteochondrosis is no exception in this regard. This pathology, which affects the intervertebral discs, is the result of long-term degenerative-dystrophic processes. In most cases, it is impossible to determine exactly what triggered the development of the disorder. Factors that can provoke the appearance of osteochondrosis of the thoracic spine include:
- congenital or acquired deformities of the spine;
- overweight;
- overload of the spine during pregnancy;
- infectious diseases;
- hypothermia;
- metabolic disorders;
- hormonal disturbances;
- chronic stress;
- bad habits;
- connective tissue diseases;
- dysplastic changes;
- postural disorders;
- unhealthy diet;
- injuries.
Detraining negatively affects the condition of the spine. People who lead a sedentary lifestyle are more likely to suffer from thoracic osteochondrosis. Additionally, age-related changes and slowing of metabolism seen in patients over 55 years of age contribute to the development of these disorders.
Genetic predisposition can be a factor that can cause the development of pathology. The genes that create the conditions for the appearance of breast osteochondrosis have not yet been identified, but in people with a family history of cases of this disease, it is diagnosed more often.
Symptoms and signs
The clinic of this pathological condition depends on the negligent stage of the process, the level at which the intervertebral disc injury occurred, and the age of the patient. In the early stages of development, there are no specific signs, but general symptoms can occur periodically. Often, in the initial stages of development, the disease manifests itself only with the onset of cold weather or after physical overexertion. The initial manifestations of the development of osteochondrosis of the thoracic region include:
- rapid fatigue;
- back pain and pressure;
- muscle spasms;
- cold limbs.
As the disease progresses, the patient's condition worsens. Painful pains appear in the chest. Especially often they occur against the background of prolonged stay in one position or with sudden movements. Also, severe pain syndrome can appear when lifting weights. Rotating your torso can increase pain. The presence of osteochondrosis is also indicated by the appearance of dull pain in the area of the shoulder blades.
Often, osteochondrosis of the thoracic region is accompanied by the appearance of an abnormal curvature. In severe cases, the patient may develop a hump. Also, this disease can provoke the appearance of pain during deep breaths and exhalation.
When nerve roots are pinched, there is often a sensation of numbness in the upper extremities and upper body skin. Due to the violation of innervation and blood circulation, a feeling of goose bumps appears on the skin. The feet and hands are always cold. There may be sensory impairment in the extremities. In advanced cases, this disease can provoke the appearance of symptoms of damage to other organs as a result of a violation of their innervation. In the later stages of the process, you may:

- intercostal neuralgia;
- stool disorders;
- swelling;
- heartburn and nausea;
- itchy and burning feet;
- violations of the reproductive system;
- asthma attacks.
As the pathology progresses, a person's work capacity decreases. Physical activity is minimized. In the future, this disorder can create preconditions for the development of serious complications. Increases the risk of pathological fractures. The curvature of the spine leads to compression of the organs located in the chest.
With an unfavorable course, the disease progresses with an infringement of the heart muscle and a decrease in lung volume. Most often, these serious complications are accompanied by generalized osteochondrosis, in which several intervertebral discs are affected at the same time.
Degrees of thoracic osteochondrosis
The existing classification subdivides the development process of this pathology into 4 degrees. Each of them is characterized by the presence of a series of changes in the structure of the intervertebral discs, vertebrae and other elements that make up this part of the spine.
First grade
In the first degree of pathology, there are no pronounced clinical manifestations, but specific changes in the structure of the intervertebral discs can already be revealed with a comprehensive diagnosis. The annulus fibrosus, which receives less moisture and nutrients, gradually loses its elasticity. Microcracks often form in the tissues, within which the nucleus pulposus is squeezed. Displacement of the discs into the spinal canal is possible. Bumps form. There are no signs of a ruptured annulus fibrosus.
Second grade
With the transition of the disease to the second degree, the first clinical manifestations are observed. Periodically, patients experience pain and other neurological signs. By performing specific diagnoses, signs of decreased elasticity of the tissues that form the annulus fibrosus can be detected. Cartilage becomes very thin, increasing the risk of hernias. There is a decrease in the height of the intervertebral discs, due to which the structures of the spine acquire abnormal mobility.
Third degree
In the third stage, changes in the structure of the discs become so pronounced that the first signs of the development of kyphosis or scoliosis appear. Often at this stage in the process, the damaged annulus fibrosus ruptures. This phenomenon is accompanied by the exit of the nucleus pulposus beyond the disc. A developing hernia, depending on the direction of the bulge, can compress the nerve roots or the spinal cord. Severe pain and neurological disorders occur. The mobility of the spine increases, which creates conditions for injuries and fractures.
Fourth degree
With the transition from the pathology to the fourth stage of development, the structure of the intervertebral discs is so altered that they stop performing a depreciation function. The annulus fibrosus and nucleus pulposus lose elasticity. These elements begin to ossify. Due to a violation of the amortization function of the discs, the vertebrae suffer, bearing too much load.
At the edges of the vertebrae adjacent to the damaged disc, osteophytes, that is, bony growths, begin to grow rapidly. The surrounding ligaments are involved in the pathological process. They lose elasticity and no longer adequately support the spine. Also, at this stage of the development of the pathological process, the work of the muscular apparatus is disrupted.
Make a diagnosis
When signs of this disorder develop, the patient needs a consultation with a neurologist and an orthopedic surgeon. First, the doctor conducts an external examination and collects an anamnesis. Laboratory tests that are often prescribed for the diagnosis of this disease include blood and urine tests. X-rays are taken to obtain information about the presence of defects in the structure of the spine. This research reveals:
- lowering the disk height;
- jagged edges of elements;
- hernia;
- change of vertebral bodies;
- forming osteophytes and so on.
To clarify the defects in the structure of the disc, a discography is assigned. This study allows you to identify the uneven contours of the nucleus pulposus, assess the degree of destruction of the disc and the decrease in tissue density. CT and MRI scans are often done for better visualization. Considering that the clinical manifestations of thoracic osteochondrosis are similar to the symptoms of coronary heart disease, electrocardiography is often prescribed to differentiate these conditions.
Treatment options
This pathological condition requires complex treatment. First of all, patients are selected drugs that help to eliminate symptomatic manifestations and improve the nutrition of the intervertebral discs. The medication should be supplemented with physical therapy and exercise therapy. As a complement, you can use some home remedies. In addition, it is recommended to follow a specific diet.
Medications
In case of severe pain syndrome, the patient is advised to adhere to bed rest. This will reduce the intensity of the pain. To eliminate discomfort, pain relievers and NSAIDs are often prescribed. If the pain syndrome manifests itself too intensely, blockages may be required. Glucocorticosteroids are often prescribed to eliminate pain in this disease.
Chondroprotectors are prescribed to improve nutrient and water saturation of the intervertebral discs. In some cases, antispasmodics and muscle relaxants are prescribed in short courses. These medications help relieve muscle spasms. If necessary, diuretics are prescribed to remove soft tissue edema. To improve the state of compressed nerve endings, the patient needs B vitamins.
Physiotherapy and massage
Physiotherapy and massage are the most important components of osteochondrosis treatment, but they can only be used after suppression of symptoms with medication. Properly selected exercises help improve lung ventilation and strengthen the muscular corset that supports the spine.
First, all necessary exercises must be learned under the supervision of an exercise therapy instructor. In the future, the patient can exercise at home. People with this condition may be advised to take classes in the pool.
Massage helps to eliminate muscle hypertonicity and improves soft tissue nutrition. So that the procedures do not harm, they must be carried out by a specialist. In most cases, a classic massage is performed, which consists of successively rubbing, smoothing and pinching the problem area. Acupressure and segmental massage can be of great benefit. These techniques involve hitting the pain points. They help improve blood circulation and lymphatic drainage. In most cases, it is enough for patients to perform procedures 2-3 times a week.
Acupuncture
This method involves placing needles in areas of the patient's body. This method allows you to quickly eliminate muscle spasms and pain. Acupuncture procedures must be performed by a professional in this matter. If a specialist does this, the procedure will be almost painless. Acupuncture is contraindicated for people suffering from oncological diseases, mental disorders. It is not recommended to use this method to treat osteochondrosis in the presence of severe inflammatory processes.
Manual therapy
Manual therapy helps restore the correct anatomical position of the vertebrae. In addition, this method helps reduce the intensity of pain and muscle spasms. This effect helps restore the ligamentous apparatus. Such procedures can slow down the development of this pathological condition. The duration of the course of manual therapy is selected individually for the patient.
Post-isometric relaxation technique

Post-isometric relaxation procedures are a special technique that involves tensing all the muscles that surround the spine and then relaxing them.
These exercises should be performed under the supervision of a specialist who can assess the correctness of movement and the severity of muscle tension. This method allows you to quickly eliminate pain and restore normal function of muscles and ligaments.
Folk remedies
It is impossible to treat osteochondrosis only with folk remedies, since this approach can cause a worsening of the course of the disease. It is best to use a variety of herbal formulations and other natural ingredients as a complement to traditional therapies. You should get a doctor's recommendation on the advisability of using this or that folk remedy before you start using it.
Celery root
Well-cooked celery root is believed to help saturate cartilage tissue with nutrients and water. To prepare this product, you must cut 1 root well and pour 1 liter of boiling water. You need to insist on the composition for at least 8 hours. After this time, you need to strain the product and take 1 tsp. 3 times a day before meals.
Sunflower root
For the treatment of osteochondrosis of the cervical spine, a decoction of sunflower root is often used. To prepare this product, you will need about 1 glass of chopped vegetable ingredient, pour 3 liters of water. The mixture should be boiled for 3-5 minutes. After that, the agent must be cooled and taken in the form of tea for several days. To improve the taste of the drink, honey can be added to it. It is best to keep the rest of the medicine in a thermos.
Homemade ointment
A simple homemade ointment can be used for rubbing with osteochondrosis. To prepare this product, you need to melt approximately 150g of pork fat in a water bath. After that, 2 tbsp should be entered. l. natural wax.
The composition must be boiled for at least 20 minutes. After that, 1 tablespoon should be added to the heated mixture. l. fir oil. The product must be boiled for another 20 minutes. Finally, 2-3 minutes before removing the container from the heat, add 1 tablespoon to the mixture. l. ammonia. The finished composition must be distributed in jars. Store the homemade ointment in the refrigerator.
Nutrition for thoracic osteochondrosis
Patients suffering from osteochondrosis of the thoracic region need a balanced diet. A sufficient quantity of protein-rich foods should be introduced into the diet. It is advisable to regularly consume dishes that contain a large amount of chondroitin, including fish aspic, jellied meat, etc. It is imperative to introduce fermented dairy products, vegetables and fruits in the diet. Dishes should be steamed or baked. Fatty and fried foods should be avoided. It is advisable to eat food in small portions, but often. This will avoid overeating.
Aggravation: what to do?
In the acute period of the disease course, it is desirable to reduce activity to a minimum. If possible, you should avoid poses in which the pain syndrome is intensified. First aid for exacerbation of osteochondrosis involves the use of drugs that reduce the severity of edema, inflammation, and pain. The patient is advised to rest in bed. It is advisable to follow a moderate diet during this period. Only after eliminating the symptoms can exercise therapy and physical therapy begin.
Forecast
Now, this disease can only be cured in the early stages of development. With a late diagnosis, therapy aims to eliminate symptoms and improve spinal mobility. In some cases, surgical treatment is required. With an integrated approach to therapy, a person suffering from this condition can lead a complete lifestyle without experiencing pain or other neurological disorders.
Prevention
To prevent the development of this pathological condition, it is recommended to avoid lifting heavy objects suddenly. You should always dress according to the weather, avoiding hypothermia. Also, to prevent osteochondrosis, one must combat hypodynamics and control posture. As part of the prevention of this pathology, it is recommended to eat well and carefully monitor your weight.

























